Temple Court carer speaks out about problems at Covid outbreak nursing home shut down by authorities


A carer from a Kettering nursing home shut down after a major Covid-19 outbreak, in which 16 residents died, has spoken out about the poor level of care at the home.
Kelly Simkins, who worked at Temple Court in Kettering for 13 months, says she hopes the place never re-opens and is speaking out to let relatives who lost loved ones know some of what went on.
Advertisement
Hide AdAdvertisement
Hide AdTemple Court is one of 85 in Northamptonshire that has been affected by a Covid outbreak since April, but is the only one under investigation by police regarding its care practices. The home was shut down on May 15 after a joint decision by Northamptonshire’s health and social care authorities.

Kelly, who has been a carer for more than a decade, says that Temple Court, which is part of Minster Care, is the worst care home she has ever worked at and that she had constantly highlighted problems to management and the Care Quality Commission during her 13 months working there.
She says there were problems with faulty and inadequate equipment and she says that when Covid hit the home was not prepared to handle it.
She said: “There were problems before Covid. Broken slings, hoists and wheelchairs and sensory mats that did not work.
Advertisement
Hide AdAdvertisement
Hide Ad“We had no support from management whatsoever. When you went to them with a complaint it was ‘I’m busy and I will deal with it later’.
She added: “Covid is Covid, but they did not help the situation. They have not had the best interests of the residents at heart. They have not looked out for the residents. They have not supported us carers.
“I was their voice. Before Covid a lot of the residents had families who could speak for them. But when Covid happened no-one could talk for them.
“I stayed there for the residents. My job is to care. I cared.”
Advertisement
Hide AdAdvertisement
Hide AdThe mother of two says it was devastating to work at the home while elderly residents were losing their lives to the virus. She would often turn up on shift to find another resident had gone to hospital. Most would not return.
She said: “I felt heartbroken. A lot of carers had strong bonds with the residents.
“The residents were absolutely amazing. They were very challenging but that is part of the job. We were not told how they died, we would often come in for a shift and someone else had been taken to hospital.”
Kelly claims staff welfare was not a concern throughout the pandemic and after taking in 15 residents from the hospital in mid March, many of whom later sadly died of the virus, the registered manager went off sick and there was often no manager on site.
Advertisement
Hide AdAdvertisement
Hide AdStaff were given fabric face masks and told to put tissue down them to add a further protective barrier. She says for many weeks carers did not receive Covid tests and only the management were tested. She had a test on May 9, six days before the home closed, which came back negative.
She also says management carried out a series of interviews on May 8 and despite Covid being present in the home, interviewees were not given personal protective equipment.
Kelly paints a grim picture of life in the home. She said all food was frozen, even down to the soup, and that carers were not able to spend any quality time with residents as the majority of their shift was spent doing practical tasks.
She says there was an activity timetable on the wall but activities were rare. She said one resident did not have a wash or bath in 10 months and that many had bed sores.
Advertisement
Hide AdAdvertisement
Hide AdMany of the families only became aware that there was Covid in the home after their relative became ill and died and none of them were aware of the scale of the deaths that were happening.
A number have said they asked the home for updates about Covid but were told by staff that they were not at liberty to say.
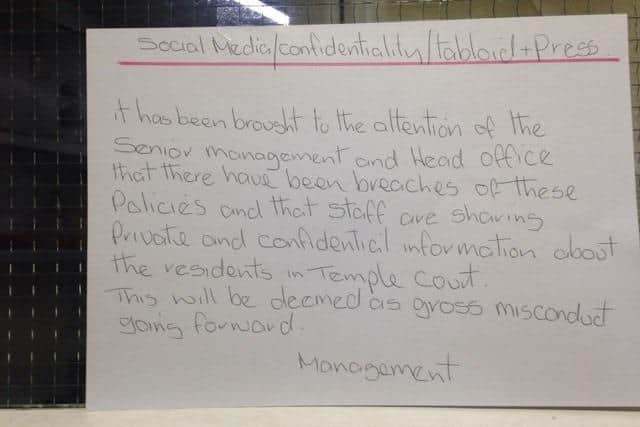
Kelly says there was a sign in the home telling staff not to speak to the media or they would face disciplinary action.
The home was closed on May 15 after a joint decision by the Northamptonshire Clinical Commissioning Group and Northamptonshire County Council’s Adult Social Care department. In the days before that surviving residents were moved out to other care homes, with some relatives only hearing about the move a day before it happened.
Advertisement
Hide AdAdvertisement
Hide AdKelly refused to speak with the CQC and NHS staff during the days they were moving out patients because she was annoyed at the way residents were being treated and also annoyed that the CQC had not responded to her earlier complaints. She walked out of her shift on May 12.
The majority of staff had their contracts terminated a week after the home closed. Kelly received a letter on May 25 saying she would be paid a week’s notice.
She said her experience at Temple Court would not stop her working in care again as it is a profession she loves.
She said: “I have worked in many amazing care homes and I will proudly be known as a whistleblower. When you are a carer you never switch off. Everything is in the best interests of those you are caring for.”
Advertisement
Hide AdAdvertisement
Hide AdTemple Court has disputed many of Kelly’s claims. It says faulty equipment was repaired or replaced; Covid tests were given to priority staff who were dealing with the Covid patients; the resident who was not washed for 10 months had refused; the frozen food was nutritious; there was oversight from an area manager when manager Tina Dauncey went off ill and that the staff interviewed on May 8 were done so under social distancing rules and were not put at risk.
A spokesman said: “The home was assessed last year as requiring improvement and significant investment was made in both the management team and physical environment, with the sole aim of improving the quality of care and experience for residents. Huge progress was made over a number of months and this was recognised in an extremely positive report by the local authority in late January.
“Unfortunately, the effects of the Covid-19 pandemic, which struck both residents and staff, caused the home to become overwhelmed during March and April. Despite assistance from NHS nurses and the local safeguarding partnership, standards of care continued to diminish and the home closed in May.
“A member of staff was removed from shift for poor conduct and behaviour towards the professionals supporting Temple Court during its most challenging period.”
A CQC spokesman said: "
Advertisement
Hide AdAdvertisement
Hide AdMs Simkins used CQC’s online feedback form on the evening of 19 May 2020 to provide information about the moving of people from the service. Inspectors spoke to Ms Simkins by telephone on 21 May 2020 and, with her agreement, information she provided was passed to the local clinical commissioning group.
Inspectors have subsequently telephoned Ms Simpkins to discuss her concerns further, but have had no response.
In addition to the contact from Ms Simkins, CQC received anonymous concerns about Temple Court. These contributed to our ongoing monitoring of the service and our decision to inspect it in on 12 and 13 May 2020. The findings of this inspection will be published as soon as possible."
The police investigation is expected to take many months.
Did you have a relative a Temple Court? If so, you can contact reporter Sarah Ward at [email protected]